A capitalisation study of the impact of a community based psychosocial interventions within the AMAL project in Libya-HI Retour vers les opportunités
Humanité & Inclusion (Handicap International )
Lance Appel à candidaturesÉchéance
30 Septembre 2021 Il y a 4 ans
Partager l'opportunité sur
Détails de l'opportunité
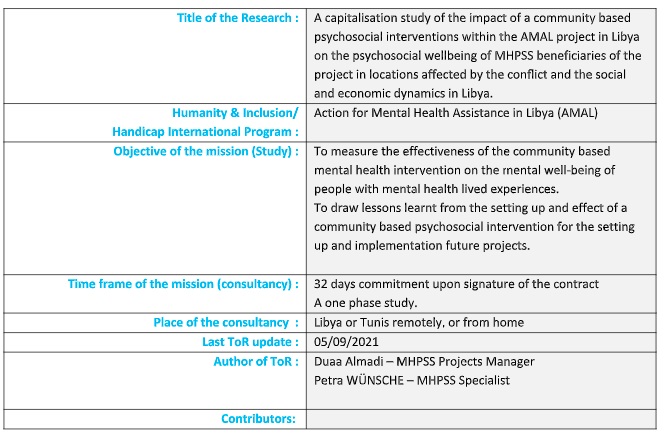
- SUMMARY OF THE MISSION AND STUDY
- GENERAL CONTEXT
People suffering from mental health problems can be found everywhere in the world, in every community and across all age groups, regardless of living standards prevailing in their country. Whereas 14% of the global burden of disease is attributed to these disorders, the majority of the affected people – of whom 75% live in low-income countries – cannot receive the treatment they need (WHO, 2017). According to the WHO, depression is the primary cause of morbidity and incapacity, and more than 300 million people globally currently live with this problem. In regions where HI operates, strengthening community-based resilience mechanisms has become a prime lever of change leading towards psychosocial improvement and greater respect for the basic rights of the populations concerned. Our interventions aim primarily at meeting the needs of persons living with mental health problems (psychosocial distress and/or mental health disorders) in order to minimize the risk of social judgement, whether this judgement manifests in the form of discrimination, stigmatization, exclusion or social isolation. With this intention, HI has over the past 27 years been working in more than 25 countries where it has run mental health and psychosocial support programmes. More specifically, HI has since 2014 been implementing the “Action for Mental Health Assistance in Libya” a mental health psychosocial support programme in Libya financed by the European Union (DG-NEAR) for the years (December 2018 – December 2021)
- LIBYA CONTEXT
Context of Libya
Since the fall of the regime of Gaddafi in 2011 and renewed conflict since 2014, the political and economic situation in Libya has become extremely fragile. Health services in Libya have gradually collapsed due to depleting human resources, equipment and medicine as well as a gross lack of investment in the sector. The population’s health and social well-being has been severely impacted as a result. With 193,581 current internally displaced persons (IDPs) and 382,222 persons returned to their area of origin in the last two years, the capacity of service providers is challenged by repeated influxes of new patients. In addition, the country is facing a migration crisis with 54,416 registered refugees and asylum seekers and an estimated 662,248 migrants present in Libya today, adding another layer of complexity to the humanitarian context.
UNOCHA estimated that the number of people in need of health services in Libya in 2018 to be 1.1 million, among them 16% IDPs, 19% returnees, 36% non-displaced and 30% migrants or refugees. 44% were female and 56% male. In terms of age groups, the majority of the people in need were assessed to be adults (61%), 33% of children and 6% elderly. Whereas, returnees were reported by REACH to be the group with the highest difficulties to access adequate healthcare (54%) as they usually return to conflict-affected areas where basic services are no longer functioning. Furthermore, 24.9% of all assessed households reported at least one member displaying two or more signs of psychological distresses, 46.7% of IDP households and 39% of returnee households (compared to 23.5% of non-displaced households).
The Mental Health System in Libya
The Mental Health/Psychosocial Support (MHPSS) 4W assessment conducted in Libya in 2017 states that “Mental Health is a chronically neglected field in the country with many longstanding problems that predate the conflict that started in 2011, including underdeveloped community and specialized services, shortage of qualified workforce, lack of facilities, social stigma towards people with mental illness and funding marginalization”. In addition, the current and long-lasting violence in the country is believed to further increase the proportion of the population in need of mental health and psychosocial support, requiring a combination of immediate and longer-term interventions.
The MHPSS 4W mapping identified a total of 190 organizations, amongst them 16 that deliver MHPSS services, programs, and activities for communities across Libya. The most common activities provided were general services to support MHPSS, psychological interventions, and specialized clinical management of mental disorders. However, some activities linked to information dissemination, community mobilization, community support, safe spaces, psychosocial support in education, inclusion of psychosocial support in other sectors, case focused psychosocial work, and non-specialized management of mental disorders were also reported. The report stated a lack of information regarding the quality of the services provided by all implementing organisations.
Mental health service provision is highly centralized in Benghazi, Tripoli and Misrata, difficult to access and of limited quality. In addition to the two mental health hospitals, Al Razy Psychiatric Hospital in Tripoli and Benghazi Psychiatric Hospital, there are 6 mental health outpatient facilities (one in Al Wahat/Ajdabia, two in Misrata, two in Tripoli and one in Al Jabal Al Gharbi). Two are in mental health hospitals, two are in general hospitals and two are in polyclinics. In parallel there are a number of private clinics, often run by professionals working in the public hospitals, but that are not accessible to the most vulnerable part of the population primarily due to financial barriers. All in-patients from the two mental health hospitals were discharged in 2014 mainly because of the lack of qualified health professionals (psychiatrics, psychologists, and nurses). A high number of qualified foreign health professionals left the country during the 2014/2015 conflict. Provision of mental health care in Libya is essentially based on prescription of drugs, and counselling and psychotherapy services are rare. In addition, psychotropic medicines are not always available and often not affordable to people with low income.
- ABOUT THE PROJECT: Action for Mental Health Assistance in Libya (AMAL)
Logical framework of AMAL
For HI, a person’s mental health depends not only on their individual characteristics but also on community, social and political characteristics. The objectives of a community-based, inclusive mental health project such as the one proposed are:
- To ensure the emergence of a community-based development process, i.e. the development of local networks, structures for promoting health, prevention actions, local government policy;
- To build organizations’ capacities (of professionals and of people with disabilities);
- To implement and/or strengthen social inclusion and equal opportunities policy.
The overall objective of the project is therefore to allow the most vulnerable people in Libya (adults, adolescents and children) from host communities, those internally displaced, returnees and migrants, suffering from mental health disorders/psychosocial disabilities to regain or to preserve good mental health by accessing quality interventions at community level, primary health care level, and secondary and tertiary level.
Target group of the action
The final beneficiaries of this action are children, adolescents and adults with mental health disorders/psychosocial disabilities living in the three major cities of Libya – Tripoli, Benghazi and Misrata – and their caregivers, including all status of persons: host community members, IDPs, returnees, refugees and migrants. Due to social stigma, difficulty of access and lack of MHPSS services in Libya at all levels of service delivery (community, primary, secondary and tertiary level) the needs of these people are largely uncovered. Target groups of the action;
- People with mental health disorders/psychosocial disabilities (final beneficiaries) through the implementation of actions at the community level: awareness campaigns and sessions on the most common mental health disorders and access to mental health care to tackle the issue of stigma; direct provision of services at community level such as home visits, individual and group sessions on psychoeducation, low-intensity psychological interventions (such as Problem Management + (PM+); Group Interpersonal Therapy (ITP) for depression, developed by WHO), parenting skills trainings, peer to peer groups. Based on HI current projects, special attention will be paid to provide access to MHPSS to people with functional limitations and to integrate physical and psychosocial rehabilitation. Victims of explosive hazards are also a target group for HI in Libya, linking its current Mine Action activities in the provision of victim assistance services.
- Health professionals (junior and senior, non-specialized and specialized), through a capacity building component: psychosocial workers, nurses, family doctors/GPs, psychologists and psychiatrists. All these professionals, either newly graduated or already active within public health facilities (Primary Health Care Units, Primary Health Care Centres, MHPSS departments of General Hospitals, MHPSS Specialized Hospitals), will benefit from training provided by NEBRAS and HI on clinical and community intervention in mental health.
- The Ministry of Health (the Directorate of Primary Health Care Services, the Directorate of Hospital Services, the Directorate of International Cooperation and the Directorate of Nursing and of Human Resources, the Mental Health Department of the National Centre for Disease Control under the umbrella of the Ministry of Health, local departments of the Ministry of Health in Greater Benghazi and Tripoli, selected services (PHC Units, PHC Centers), MH departments of General Hospitals, MH Specialized Hospitals). Selected public health facilities will benefit from increased technical capacities of their staff (see target group above), but also from better working procedures, referral pathways, and guidelines regarding care of people with mental health disorders/psychosocial disabilities.
- ABOUT THE STUDY:
Why this study and why it is needed?
Research in the MHPSS sector is a missing piece. There has been a great need to develop a research agenda to strengthen mental health and psychosocial support in humanitarian and development settings; prior research in this area has had limited inputs from practitioners especially in Libya. If HI has collected lots of anecdotal evidence about the added-value of its MHPSS interventions, it is still extremely challenging to demonstrate effectiveness of its Strategy and interventions. HI needs to build the evidence around its MHPSS Community-based Interventions with robust methods and clear guidelines. HI needs to understand what worked well and what did not work well in a country Libya which is a new MHPSS field of intervention. Finally, HI needs to add evidence in the global MHPSS sector.
The value and use of this study:
- The results will be used to (re)orient the intervention in Libya
- The used quantitative and qualitative tools and methods will feed a more global reflection on Monitoring and Evaluation of existing and new MHPSS projects within HI
- The Outcomes and Learnings will be shared at local, regional and international level:
- Operational level: Share with National Mental Health (PHCI) and MHPSS TWG, other peers from the civil society, the users’ movements and the services providers the learnings and challenges in the implementation of such a project.
- Research level: to benefit MHPSS practitioners in working on Libya and global MHPSS issues in understanding MHPSS access barriers and conduct further research of their own
- Advocacy purpose: Show policy makers, decision makers and donors that it is possible to build effective community based MHPSS intervention (and how) with a strong focus on the participation of people with lived mental health experiences.
- OBJECTIVE AND STRUCTURE OF THE STUDY
As part of AMAL project, HI has implemented low intensity psychosocial community based interventions, directly through HI team of psychosocial workers and indirectly through training of MoH and CSOs staff. The study will explore the practices implemented in order to generate robust evidence in the identification of the impact of such practices on MHPSS beneficiaries and aid the future development of contextually sensitive MHPSS programmes to better respond to the needs of populations affected by the humanitarian crisis.
This study aims to reveal:
- Description of the project set up and its activities and difficulties faced
- patterns of profiles of beneficiaries
- impact of such practices / approach on the beneficiaries’ mental health conditions and psychological well-being
- needs for changes in practices as well as recommendations for future programming
The methodology adopted to conduct this study will be both, quantitative and qualitative: :
- Desk review of project documents, reports of AMAL
- Analysis of the practices implemented during the programme through interview with key informants among HIs psychosocial workers and of MoH and CSOs staff trained by HI
- Analysis of HI’s beneficiaries database to understand better the profiles of beneficiaries and the difficulties they have been or are facing in such context;
- Analysis of individual data, through review of beneficiaries’ files and interview
- Capitalisation report
Location
The study will take place in Tunis or remotely with possibility to access the project implementation areas by the time of selection and contracting.
Ethics and Confidentiality
The ethical principles adopted by HI can be transposed into 8 interdependent recommendations specific to the data management:
-Guarantee the security of all the partners involved;
-Ensure a person/Community-centered approach;
-Obtain the subjects’ free and informed consent;
-Ensure referral mechanisms are in place;
-Ensure the security of personal and sensitive data at all stages of the process;
-Plan and guarantee the use and sharing information;
-Ensure the expertise of the teams involved and the scientific validity of the activity;
-Obtain the authorization from the relevant authorities and organize an external review of the proposed Research.
Please refer to: Studies and Research at Handicap International: Promoting data ethical management, Collection: Guidance Note, September 2015
Specific challenges and constraints
CHALLENGES
HI and its consults have had issues accessing Libya and project locations. HI MHPSS team based in Tunis will ensure proper presentation of the structure and means of communication with field staff including partners.
KNOWLEDGE TRANSLATION
Following the study and the final workshop and products, HI will implement regular communication on the results and lessons learnt with its regional/HQ offices, MHPSS TWG, and donors to feed our practices in the relevant programmnes in Libya.
Set up of the study
In close collaboration with HI, the consultant will ensure the planning, the implementation including all final products, are fully implemented and are corresponding to the results and timeline as per the contract and its annexes.
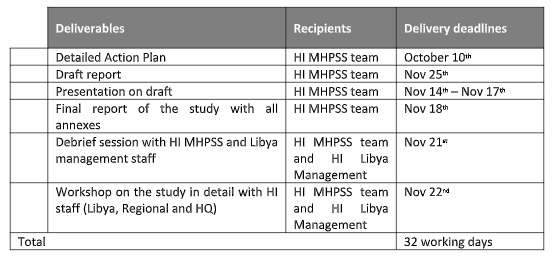
Time Schedule
HI expects this study to start in October 2021 for 32 days as explained above. This means obtaining all prior authorizations. The research should be completed by end of November 2021 with workshop and meeting to be conducted by first week of December 2021.
Mechanisms for communication and monitoring between the consultant and Handicap International
This study will be monitored by HI teams and partners in Tunis and Libya, HI MHPSS Project Manager, MHPSS Specialist in Tunis, and the Operations Manager in Tunis.
- PROFILE NEEDED
Requested profile
The call will be open to Mental Health professionals with a proved experience in research
Expertise
- Mandatory
- Minimum: Diploma or MA in psychology/social sciences
- Experience in MHPSS Community-based approaches in development settings
- Familiar with the cultural context in Libya or post-conflict intervention would be a strong asset
- Proven and recognized experience in methods of data collection, treatment and analysis (quantitative and / or qualitative and / or secondary data)
- Knowledge of software and statistical analysis of quantitative and qualitative data
- Analysis, synthesis and writing demonstrated capacity (provide a list of publications)
- Ability to train and manage investigators teams
- Knowledge working languages (written & oral): English mandatory
- Desired
- Recommended experience in conducting surveys including people with psychosocial problems
- (Adaptation of tools or support of communication).
- Ability to work in collaboration with public and associative actors
- Knowledge of Arabic (written and oral) is a strong asset
L'opportunité a expiré
Cette opportunité n'est malheureusement plus disponible sur Jamaity. Visitez régulièrement la rubrique opportunités pour ne plus en rater.
Suivez Jamaity sur LinkedIn
Obtenez Jamaity Mobile dès maintenant

Publié sur Jamaity le 9 septembre 2021
Découvrez encore plus d'opportunités sur Jamaity en cliquant sur ce lien.